
Travis Kelce is one of the most famous NFL players, known for his incredible skills as a tight end for the Kansas City Chiefs. However, fans are just as curious about his personal life, especially regarding Travis Kelce wife. Over the years, there have been rumors, relationships, and speculations about his love life. In this article, we will dive deep into everything you need to know about Travis Kelce wife, his dating history, and the latest updates on his romantic life.
Who Is Travis Kelce?
Before discussing Travis Kelce wife, let’s take a moment to know more about the NFL star. Travis Kelce was born on October 5, 1989, in Westlake, Ohio. He played college football at the University of Cincinnati before being drafted by the Kansas City Chiefs in 2013. Since then, he has become one of the most dominant tight ends in the league, helping his team win multiple championships.
Is Travis Kelce Married?
One of the biggest questions fans ask is, “Who is Travis Kelce wife?” As of now, Travis Kelce is not married. While he has been in high-profile relationships, he has yet to tie the knot. However, his love life remains a hot topic among fans and the media.
Travis Kelce’s Most Famous Relationships

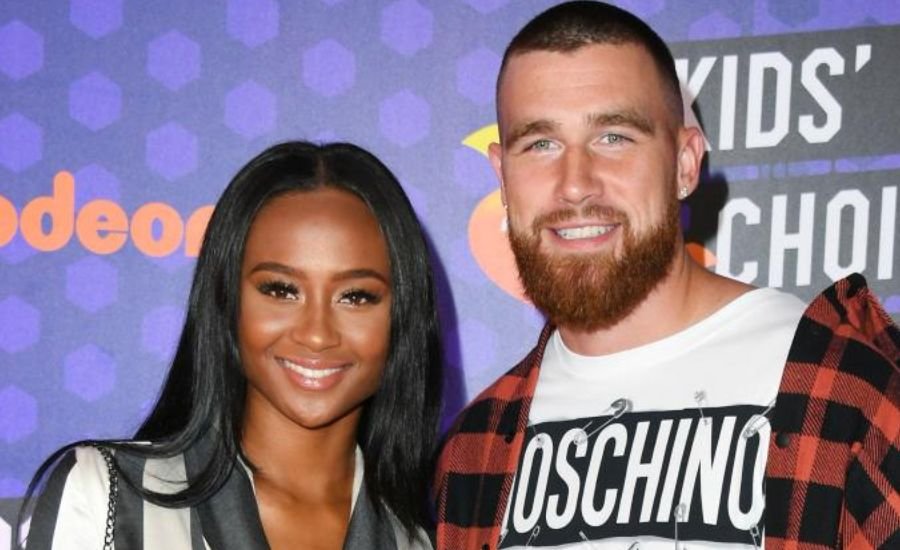
Kayla Nicole
Kayla Nicole, a well-known sports journalist and influencer, was in a long-term relationship with Travis Kelce. Their relationship lasted for several years, making many fans believe she would eventually become Travis Kelce wife. However, they broke up in 2022, leaving fans speculating about the reasons behind their split.
Taylor Swift Rumors
Recently, there have been rumors linking Travis Kelce to pop superstar Taylor Swift. While neither has confirmed a relationship, their interactions have fueled speculation. If these rumors turn out to be true, Taylor Swift could potentially become Travis Kelce wife in the future.
What Does Travis Kelce Look for in a Wife?
Travis Kelce has spoken in interviews about what he looks for in a partner. He values personality, intelligence, and a great sense of humor. If and when he decides to settle down, Travis Kelce wife will likely be someone who shares his passion for life and sports.
Travis Kelce’s Love Life in the Media
The media closely follows Travis Kelce’s relationships. From social media posts to public appearances, every detail about his love life is analyzed. Whether it’s a new girlfriend or rumors about Travis Kelce wife, fans are always eager for updates.
Read Next: Entertaincraze
Will Travis Kelce Get Married Soon?
While there is no official news about Travis Kelce wife, many believe he may settle down soon. With his career at its peak and his personal life under the spotlight, fans are excited to see what the future holds for him.
The Impact of Fame on Travis Kelce’s Relationships
Being a high-profile athlete comes with its challenges, especially in personal relationships. Many celebrities and sports stars struggle with maintaining privacy in their romantic lives. Travis Kelce wife, if and when he gets married, will likely have to deal with the pressures of fame and public scrutiny.
Social Media and Dating
Social media plays a huge role in modern relationships, and Travis Kelce’s love life is no exception. Fans analyze his Instagram posts, Twitter interactions, and public appearances to gather clues about his dating life. This adds another layer of complexity to finding and maintaining a long-term relationship.
Travis Kelce’s Family and Their Influence
Family is important to Travis Kelce, and his parents and brother, Jason Kelce, have always supported his career. When he eventually chooses Travis Kelce wife, it is likely that his family’s opinion will play a significant role in his decision.
The Future of Travis Kelce’s Love Life
As one of the biggest stars in the NFL, Travis Kelce’s personal life will always attract attention. Whether he remains single, starts dating someone new, or finally finds Travis Kelce wife, his fans will be watching closely.
Conclusion
The mystery of Travis Kelce wife continues to intrigue fans. Whether he is single, dating, or planning to get married, his love life remains a topic of discussion. As one of the biggest stars in the NFL, Travis Kelce’s personal life will always attract attention. Stay tuned for the latest updates on who might become Travis Kelce wife in the future!
FAQs
Q: Is Travis Kelce married?
A: No, as of January 2025, Travis Kelce is not married.
Q: Who is Travis Kelce’s current girlfriend?
A: Travis Kelce began dating singer-songwriter Taylor Swift in 2023.
Q: Did Travis Kelce date Kayla Nicole?
A: Yes, Travis Kelce was in a relationship with social media influencer Kayla Nicole from 2017 to 2022.
Q: Does Travis Kelce have any children?
A: No, Travis Kelce does not have any children.
Q: Who is Jason Kelce’s wife?
A: Jason Kelce, Travis’s brother, is married to Kylie Kelce.
Q: Are Travis Kelce and Taylor Swift still together?
A: As of January 2025, Travis Kelce and Taylor Swift are still in a relationship.
Q: How has Travis Kelce’s relationship with Taylor Swift impacted his popularity?
A: Travis Kelce’s relationship with Taylor Swift has significantly increased his popularity, attracting attention from fans who were more familiar with Swift.
Don’t Miss Out: Sarah-J-Maas-Net-Worth





